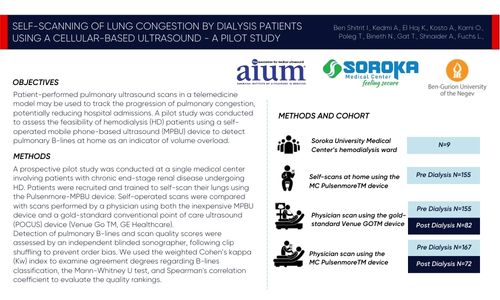
By: Ben Shitrit I., Kedmi A., El Haj K., Kosto A., Karni O., Poleg T., Bineth N., Gat T., Shnaider A., Fuchs L.,
Presented at: AIUM 2024
Objectives
Patient-performed pulmonary ultrasound scans in a telemedicine model may be used to track the progression of pulmonary congestion, potentially reducing hospital admissions. A pilot study was conducted
to assess the feasibility of hemodialysis (HD) patients using a self-operated mobile phone-based ultrasound (MPBU) device to detect pulmonary B-lines at home as an indicator of volume overload.
Methods
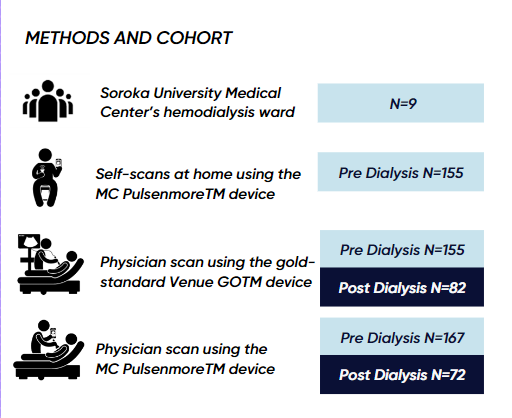
A prospective pilot study was conducted at a single medical center involving patients with chronic end-stage renal disease undergoing HD. Patients were recruited and trained to self-scan their lungs using the Pulsenmore-MPBU device. Self-operated scans were compared with scans performed by a physician using both the inexpensive MPBU device and a gold-standard conventional point of care ultrasound (POCUS) device (Venue Go TM, GE Healthcare).
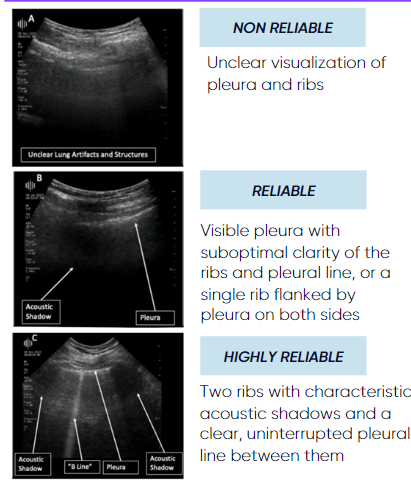
Detection of pulmonary B-lines and scan quality scores were assessed by an independent blinded sonographer, following clip shuffling to prevent order bias. We used the weighted Cohen’s kappa (Kw) index to examine agreement degrees regarding B-lines classification, the Mann-Whitney U test, and Spearman’s correlation coefficient to evaluate the quality rankings.
to assess the feasibility of hemodialysis (HD) patients using a self-operated mobile phone-based ultrasound (MPBU) device to detect pulmonary B-lines at home as an indicator of volume overload.
EVALUATION
Detection of lung B-lines and evaluating scan quality
Results
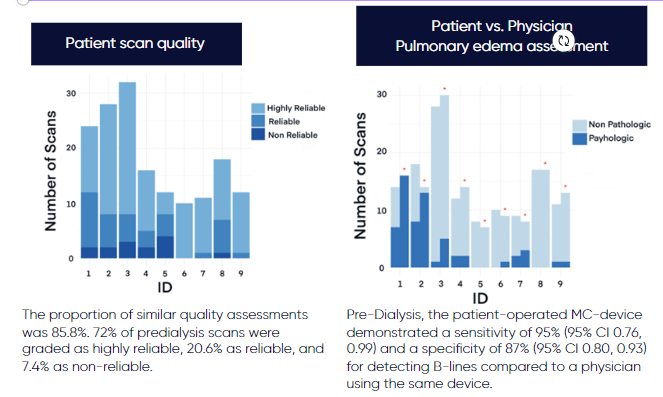
11 HD patients were recruited; 2 were excluded due to significant visual impairments ornoncooperation. During the study, 657 clips were analyzed; participants recorded 167 using the Pulsenmore MPBU device, researchers recorded 245 with the Pulsenmore-MPBU, and researchers used the Venue Go™ device for 245. Mean and median follow-up was 36.33 (SD 14.85) and 32 days (IQR 23), respectively.
Before hemodialysis (HD), patients’ self-operated scans and physician-operated scans, using the Pulsenmore-MPBU, showed substantial agreement in B-line count classification (N=146, Kw=0.64[95%CI:0.46–0.82]). Regarding the quality score rankings, there was a moderate correlation, as indicatedby a Spearman’s rs of 0.582 (N=159, p< 0.001), and a difference between operators’ scan quality when both using the Pulsenmore-MPBU device as shown by the Mann-Whitney U test result (U=12322,p=0.003).
Before HD, when a physician operated both the Pulsenmore-MPBU device and conventional ultrasound device, there was a moderate agreement for B-line count classification (N=149, Kw=0.58[95%CI:0.41–0.75]).
Additionally, for the quality score rankings, a moderate correlation was demonstrated between devices with a Spearman’s rs of 0.645 (N=155, p< 0.001), but no difference in video quality as presented by the Mann-Whitney U test result (U=13253, p=0.53).
This agreement was more substantial after HD, indicating consistent device performance with an almost perfect agreement for B-line count classification (N=57, Kw=0.81[95%CI:0.65–0.97]).
In the quality score rankings performed by a physician, there was again a moderate correlation between devices, shown by a Spearman’s rs of 0.65 (N=62, p<0.001), and similarity in video quality as presented by the Mann-Whitney U test result (U=2952, p=0.48). No adverse events were recorded during the study.
Conclusions
Patients demonstrated the ability to self-scan their lungs at home, producing scans of satisfactory accuracy and quality for detecting pulmonary congestion. This study establishes the feasibility of using the Pulsenmore-MPBU device for self-performed ultrasound scans to monitor volume overload in HD patients.
The findings suggest a cost-effective telemedicine approach that could facilitate early detection of patient deterioration, potentially reducing hospital admissions and promoting patient empowerment inself-monitoring. Such outcomes could benefit not only HD patients but also other patient groups, such as those with chronic heart failure.